

34th Annual Scientific Meeting proceedings
Date/Time: 05-07-2025 (12:00 - 12:30) | Location: Marble Hall
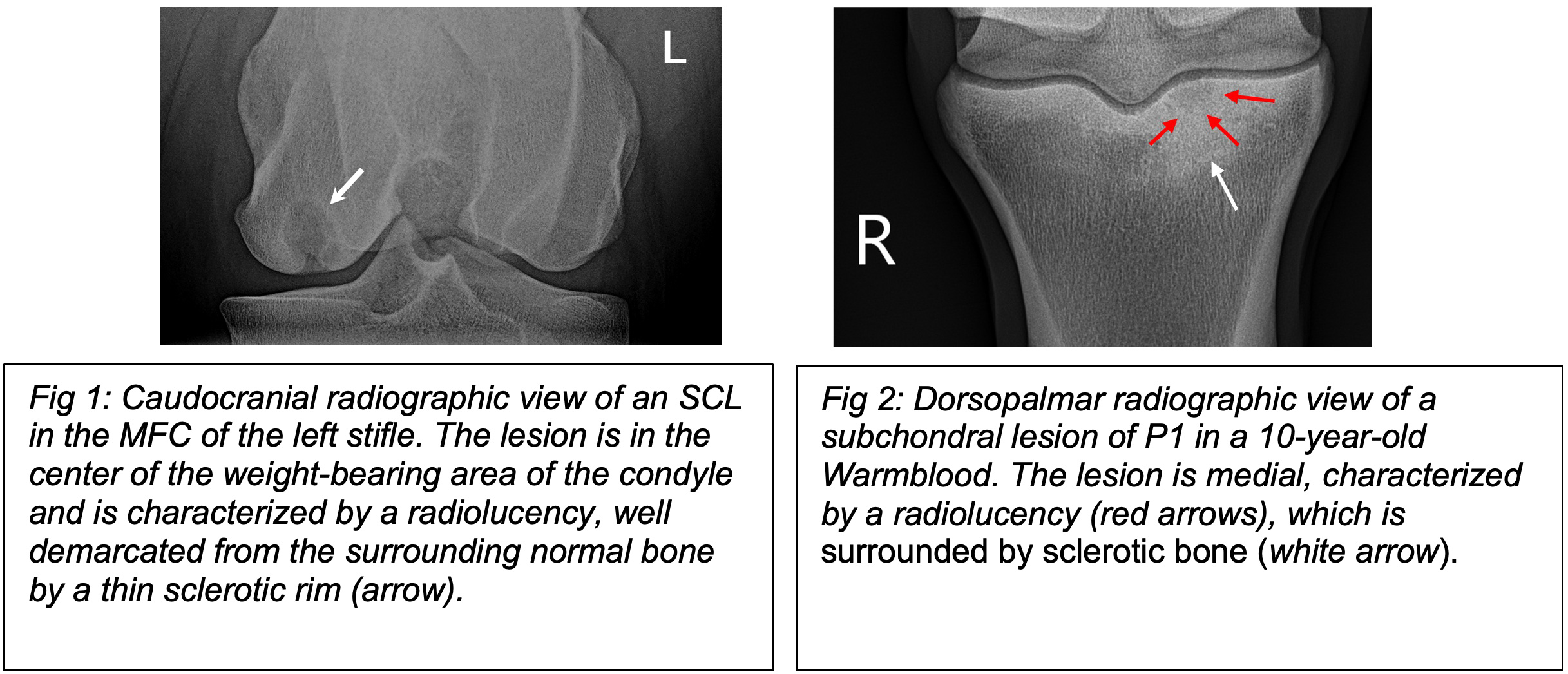
In this presentation, two different pathologies are described. The first are the classical subchondral cystic lesions (SCLs), which are typically found in the medial femoral condyle (MFC) as well as in other bones like in the proximal, middle and distal phalanx. These lesions are usually well-defined, rounded lucencies with marginal sclerosis (Fig.1). The second type are the subchondral lesions, also known as subchondral lucencies or osseous cyst-like lesions (OCLLs), resulting from bone trauma, which appear as areas of demineralization in the subchondral bone. These lesions present as irregular, indistinct regions of reduced bone density (Fig. 2).
Surgical treatment is the therapy of choice when an SCL or OCLLs causes lameness, especially in cases refractory to conservative treatment.1 In young horses intended for sale or athletic performance, surgery may be indicated prior to the onset of lameness to take advantage of the superior bone healing capacity of younger animals, to prevent cyst enlargement and the development of secondary degenerative articular changes. Surgical treatment options for SCLs and subchondral lesions are the intralesional placement of an absorbable osteoconductive implant through a transcortical approach,2 translesional placement of a cortical screw,3 or lesion debridement using either a transcortical2,4 or an arthroscopic approach,5 followed by grafting techniques.
Placement of an Intralesional Absorbable Implant through a Transcortical Approach
In this technique, a composite absorbable implant is inserted via a transcortical approach into the SCL or subchondral lesion after debridement. As the implant is reported to be bioabsorbable, biocompatible, and osteoconductive,2 the goal of the procedure is not only to resolve lameness but also to promote bone healing, thereby improving the radiographic appearance of the defects.2 The absorbable implant should be positioned within the SCL and, in case of OCLLs, as close as possible to the lesion, just beneath the articular cartilage. Ideally, the connection between the joint and the cyst cavity should be sealed by the implant. For this reason, precise drilling is essential, and the procedure must be performed under radiographic, fluoroscopic, or CT guidance (Fig.3).
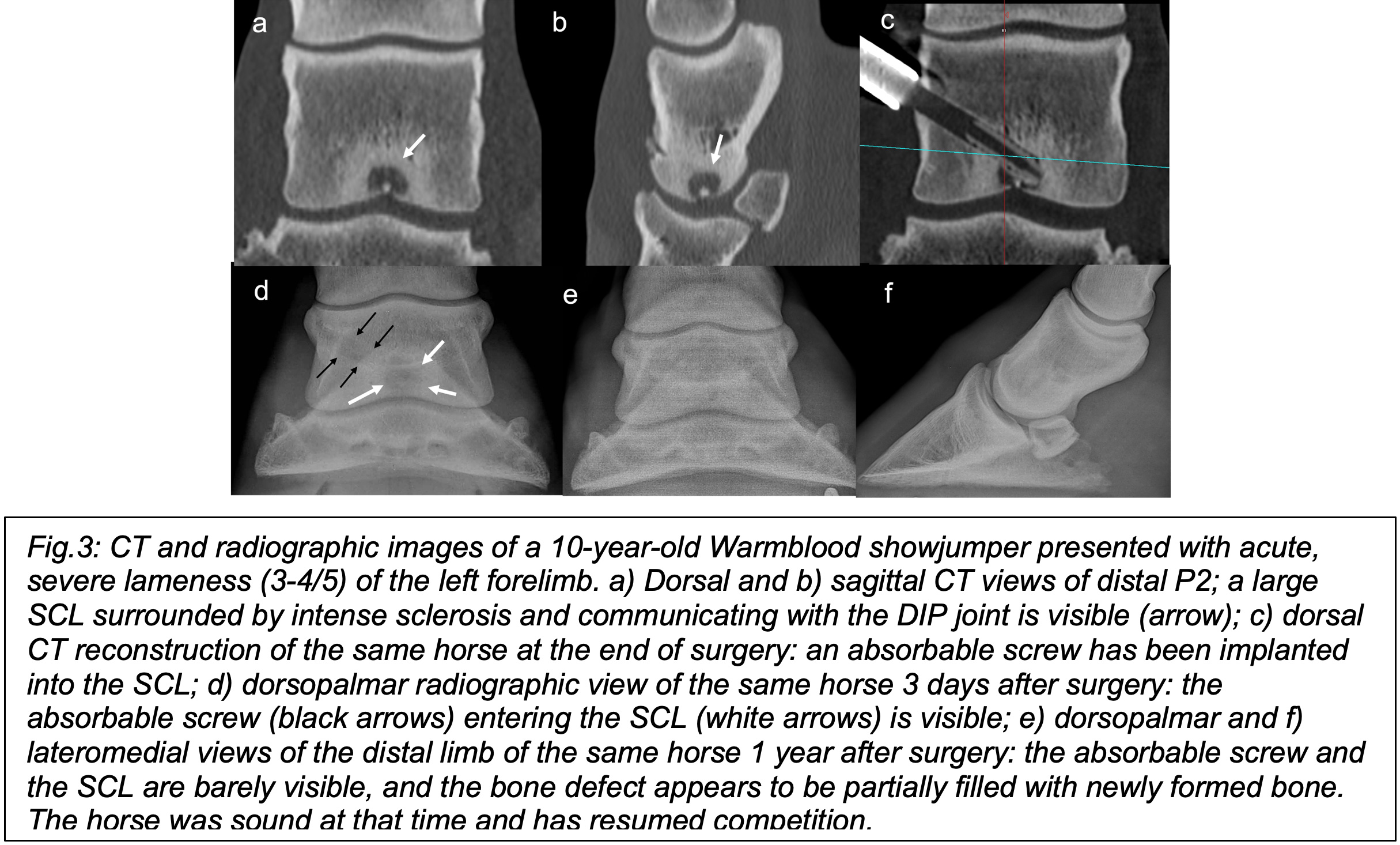
In one study, 36 out of 38 horses were sound 120 days after surgery, with an overall radiologic healing rate of 77%.2 Since then, absorbable implants have been increasingly used to treat SCLs in horses, and several studies have reported their outcomes.6,7
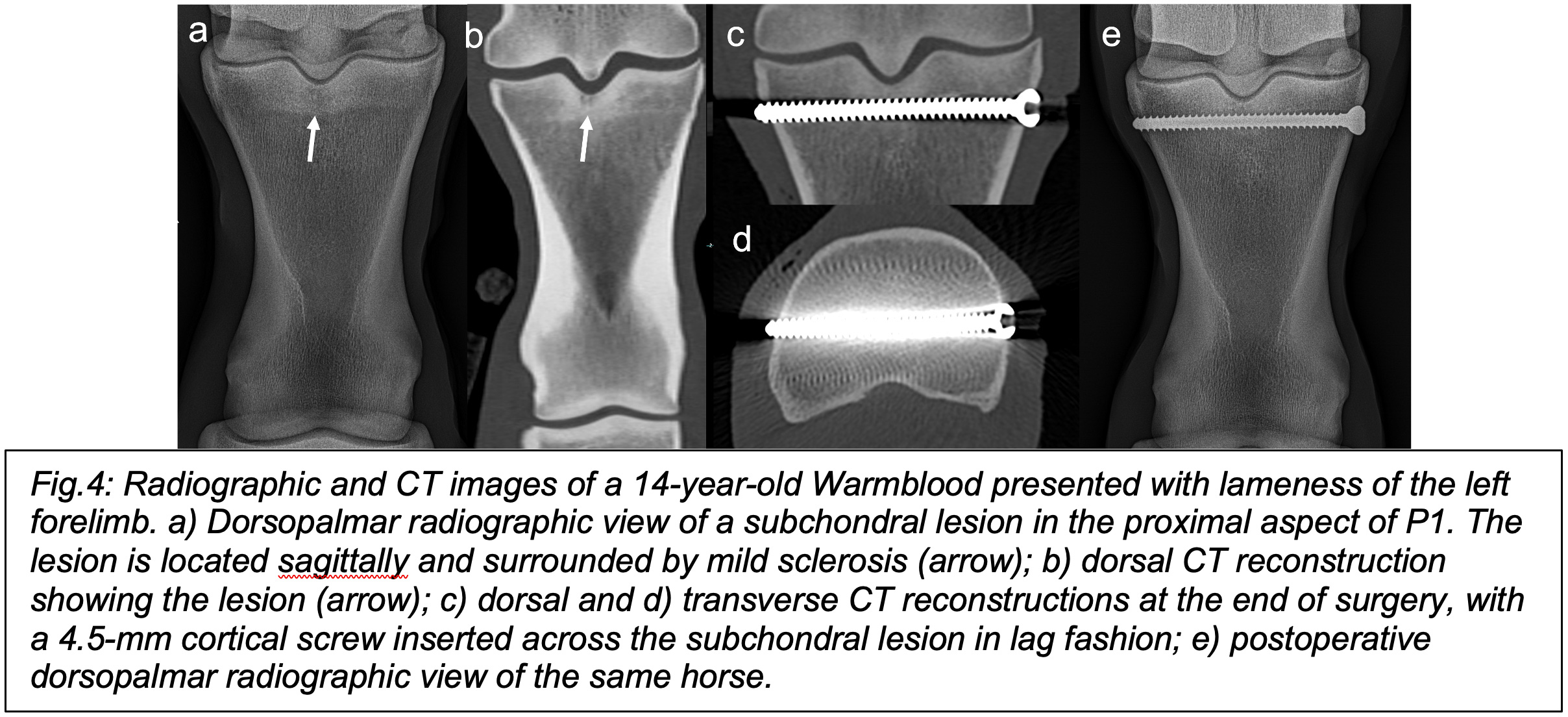
Placement of a Cortical Screw
Some authors have hypothesized that a cortex screw inserted in lag technique across a cystic lesion might promote bone formation in the SCL while preserving the overlying articular cartilage.3 In one study, 20 horses with lameness attributable to a SCL in the MFC were treated with a transcondylar 4.5 mm cortical screw inserted in lag fashion without debridement of the lesions. By 120 days, lameness was eliminated in 15 horses, and the area of the SCL had decreased by 50% or more.3 Treatment was less successful in horses older than 3 years of age.3 Compared to arthroscopic debridement, this technique has the advantage of avoiding the removal of articular cartilage. It is unclear whether, in regions such as the MFC, a 4.5mm transcondylar cortical screw can be inserted in lag fashion and whether this technique can lead to reliable healing of the SCL.8
Translesional placement of a cortical screw is a viable option for OCLLs of the sagittal groove in proximal P1. In fact, these lesions usually have a traumatic etiology, are associated with chronic stress-induced bone remodeling, and in almost one-third of the cases, a concomitant fissure line is present when evaluated on CT (Fig.4).
Debridement of the SCL using either a transcortical or an arthroscopic approach
Arthroscopy allows a thorough debridement of SCLs of the MFC, of the distal MCIII/MTIII, and essentially all lesions that are arthroscopically accessible. In recent years, an increasing number of techniques focusing on minimally invasive transcortical approaches have been developed to enable thorough debridement of lesions while preserving the cartilage overlying the SCL Furthermore, the majority of SCLs in the distal limb are not accessible via an arthroscopic approach. Careful planning and radiographic, fluoroscopic, or CT guidance are essential. Although simple debridement and exposure of the subchondral bone promote some migration of multipotent mesenchymal stromal cells (MSCs), this effect is minimal, and more advanced grafting is generally indicated for deeper lesions. Over the years, cancellous bone grafts, autologous osteochondral grafting (mosaic arthroplasty), tricalcium phosphate granules, parathyroid hormone, autologous chondrocyte implantation, and bone morphogenetic protein-2 have been used as grafts after debridement of the cystic cavity, often with favorable preliminary results.
Although no randomized studies have compared different methods and there is still no consensus on the optimal treatment, the authors believe that transcortical drilling of the SCLs and debridement of the lesions, followed by filling with a resorbable screw, appears to enhance bone healing and improve prognosis, particularly in young animals.8 Regarding lesions of the sagittal groove of proximal P1, a cortical screw in lag fashion is probably the treatment of choice to stabilize the bone.
References
- Jackson MA, Ohlerth S, Brink P, et al. Treatment of subchondral cystic lesions (SCLs) with parathyroid hormone peptide (PTH1-34)-enriched fibrin hydrogel in three different concentrations: A dose-blinded, randomised study. Equine Vet Ed 2020:121-128.
- Ravanetti P, Lechartier A, Hamon M, et al. A composite absorbable implant used to treat subchondral bone cysts in 38 horses. Equine Vet J 2022;54:97-105.
- Santschi EM, Williams JM, Morgan JW, et al. Preliminary investigation of the treatment of equine medial femoral condylar subchondral cystic lesions with a transcondylar screw. Vet Surg 2015;44:281-288.
- Jackson MA, Ohlerth S, Furst AE. Use of an aiming device and computed tomography for assisted debridement of subchondral cystic lesions in the limbs of horses. Vet Surg 2019;48:O15-O24.
- Smith MA, Walmsley JP, Phillips TJ, et al. Effect of age at presentation on outcome following arthroscopic debridement of subchondral cystic lesions of the medial femoral condyle: 85 horses (1993--2003). Equine Vet J 2005;37:175-180.
- Ravanetti P, Kuhnle C, Lechartier A, et al. An Extra-Articular Surgical Approach to Subchondral Bone Cysts in the Humeral Head and Talus in Two Horses. J Equine Vet Sci 2022;118:104092.
- Ravanetti P, Ziucca E. Subchondral cystic lesions of distal phalanx in young and mature horses: A new surgical option. Equine Vet Ed 2024;00:1-10.
- Perez-Nogues M, Manso-Diaz G, Spirito M, et al. Treatment Comparison for Medial Femoral Condyle Subchondral Cystic Lesions and Prognosis in Yearling Thoroughbred Racehorse Prospects. Animals (Basel) 2024;14.